Renal Nutrition
Pentec Health is the leader in therapies and support services designed to support patients requiring complex care and their care teams. With unsurpassed expertise, extensive experience, and empathetic compassion, we enable complex care regimens to feel simple. Driven by an uncompromising focus on healing and condition management, our services often intertwine for individualized care, based on the specific needs of each patient.
Why is Nutrition So Important During Dialysis?
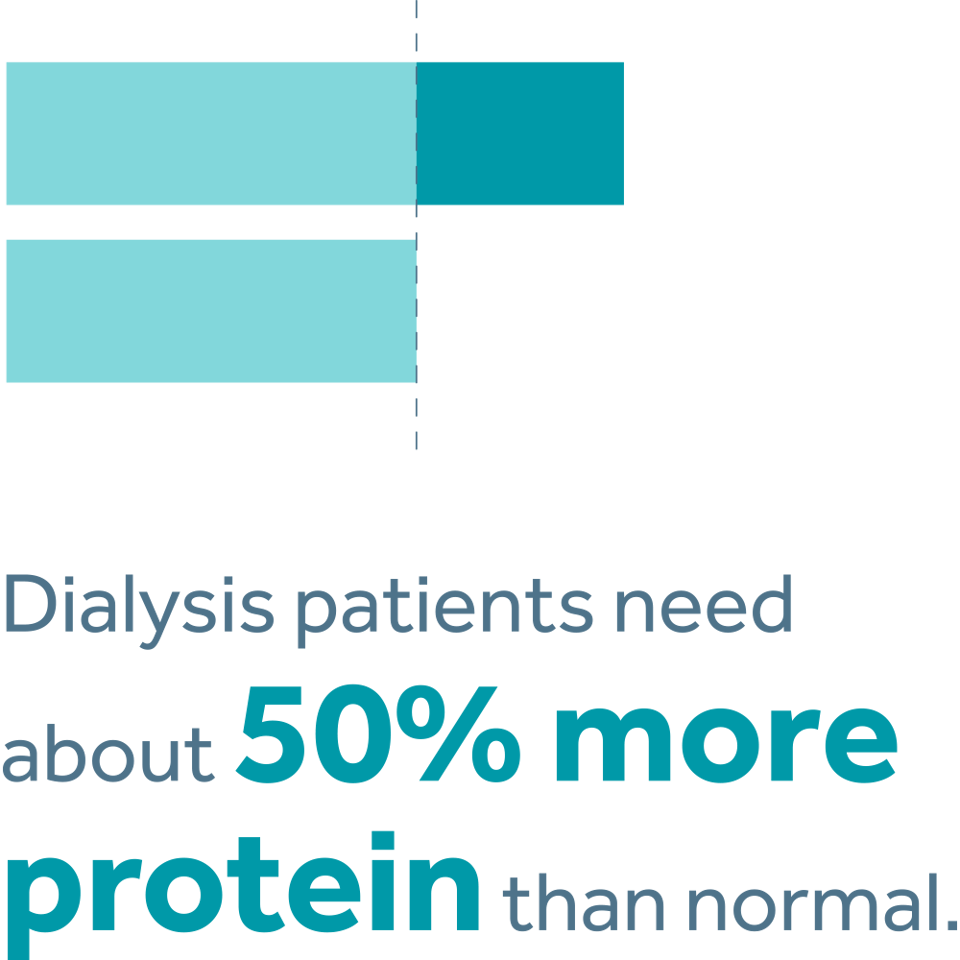
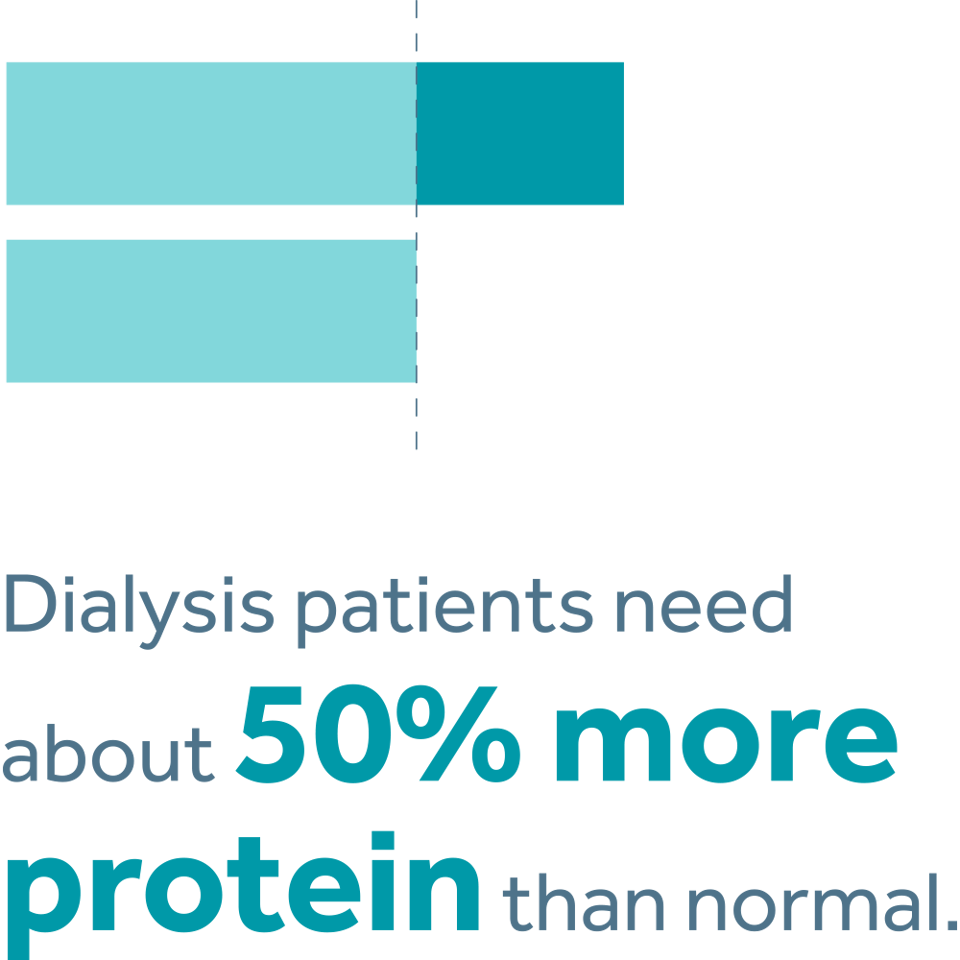
When you are on dialysis, your protein and calorie needs are higher. In fact, dialysis patients need about 50% more protein than normal. Even if you follow your dialysis diet very carefully, you may still have a hard time getting vital nutrition through food and dietary supplements alone. Furthermore, during dialysis you may experience poor appetite, nausea, vomiting, or diarrhea. This can lead to low protein levels, malnutrition, and/or weight loss. As a result, you may not feel your best and have difficulty tending to your daily activities.
What is IDPN/IPN Therapy?
In 2008, with a thorough understanding of many unmet needs for protein malnourished HD patients, our nationally recognized expert in IDPN worked to solve the tolerance issues associated with this therapy. Through her experience and discussions with clinicians, she recognized that the essential issue was composition problems inherent in traditional IDPN solutions, which caused many side effects including nausea, vomiting and chills. Her experience and expertise lead to the creation of newer, better tolerated IDPN solutions for malnourished hemodialysis patients.
The introduction of IDPN and IPN therapy was the shift in paradigm that patients and clinicians needed. With dextrose greatly reduced and lipid removed with adequate protein provision maintained, these new weight-based solutions had several advantages for both patients and the RN administering them.
Eileen Moore, CNSD, R.D., L.D.
Eileen Moore, Pentec Health's former Clinical Liaison Director-Renal Products, is a nationally recognized expert on IDPN and is the inventor of Pentec’s unique IDPN therapy for malnourished hemodialysis patients. As a renal clinician, she had many patients who did not respond adequately to standard approaches of liberalized diet and oral supplements. For these patients, protein malnutrition remained a significant problem requiring treatment with IDPN therapy. In the dialysis center and in patients dialyzed at home, she witnessed first-hand the problems they experienced with traditional IDPN solutions prompting a strong desire to find possible solutions.
Her years of experience in a tertiary care trauma hospital advising and monitoring patients requiring partial and total nutrition support allowed her to determine composition problems inherent in these traditional IDPN solutions. When coupled together, the experience and expertise led to the creation of newer, better tolerated IDPN solutions for malnourished hemodialysis patients.
What Matters Most
See How Real Patients on Dialysis Benefited from the Nutrition They Received from IDPN/IPN Therapy
Select a story to watch a short documentary about each patient's experiences, and read more about how IDPN/IPN Therapy made a real difference.
Upcoming Webinars
Choose a date to sign up for a seat. These update regularly, so check back for more.
New Insights into Sodium Balance, Sodium Storage and PEW
This focused journal article review is part 2 of our 3-part webinar series on facilitating fluid balance and CKD. Topics will include newer research related to sodium storage, sodium balance and the protein energy wasting process. Interventions to facilitate sodium balance will also be discussed, including a review of practical education tips to assist patients in achieving optimal sodium intake.

Proudly Quality Accredited
National Quality Approval
The Joint Commission

Accredited Practice Transition
Program With Distinction
American Nurses Credentialing Center
By using this website you accept our privacy policy. Choose the browser data you consent to allow:



